By: Amy Raymond, PMP, PhD, Executive Director Therapeutic Strategy Lead, Cellular and Genetic Medicines
On November 16, the British regulatory body, Medicines and Healthcare products Regulatory Agency (MHRA) approved exagamglogene autotemcel (exa-cel) to treat severe sickle cell disease for patients ages 12 and up, becoming the first gene editing treatment to receive regulatory approval. Casgevy, the commercial product formerly known as exa-cel, is administered by taking stem cells out of a patient’s bone marrow and editing a gene in the cells in a laboratory, with the modified cells then infused back into the patient after conditioning treatment to prepare the bone marrow.
In June 2023, the U.S. Food and Drug Administration (FDA) announced its acceptance of the Biologics License Application (BLA) for exa-cel. In recognition of the unmet need and medical urgency for innovative therapies in the sickle cell space, the FDA granted exa-cel Priority Review, with a formal decision expected by December 8, 2023.
Why is Casgevy a Breakthrough Gene Therapy for Patients with Sickle Cell Disease?
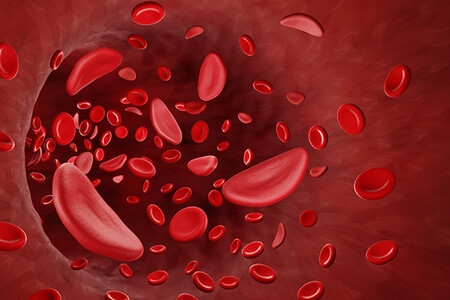
In trials, Casgevy was shown to help prevent episodes of debilitating pain, known as vaso-occlusive crises, that often plague patients affected by sickle cell disease. Due to inherited genetic mutations, the red blood cells of patients with severe sickle cell disease become misshaped and jagged, leading to obstructed blood vessels, intense pain, damaged organs, and other serious complications such as stroke. Throughout their lives, these patients routinely need emergency care, including powerful pain management and transfusions.
The treatment was effective for 29 of 30 participants affected by severe sickle cell disease for over 18 months, significantly improving the patients’ quality of life. Vertex Pharmaceuticals, the company that developed the treatment in partnership with CRISPR Therapeutics, has given exa-cel recipients a platform to share their experience with the product, enabling first-person insights capturing the potential benefit this gene editing therapy could have for the tens of thousands of patients in the U.S. sickle cell disease community and the millions around the globe who suffer from this genetic illness.
While it’s exciting to see such positive results, the novel treatment mechanism was the subject of expert discussion at the recent FDA Advisory Committee. The committee of independent advisors — leaders in their fields — was asked to consider only safety considerations related to gene editing.
One concern addressed by the committee was the oversight of “off-target,” or unintended, genetic changes that could conceivably result from any gene editing treatment, potentially causing long-term health problems. While current technologies do not support exhaustive analysis of each treated patient, advisors noted this was the most comprehensive evaluation of off-target potential ever performed. The Advisory Committee was not asked to assess the clinical benefit of exa-cel or whether the FDA should approve the application but did provide positive feedback. Long-term follow-up data will continue to be collected, providing invaluable insights into the safety and durability of Casgevy.
What Does This Approval Mean for the Future of Gene Editing?
The CRISPR technique was first published in 2012, outlining a method to harness the previously underappreciated bacterial immune system. From describing this technology to approving its first standard of care treatment in roughly a decade is a never-heard-of-before timeline. We expect Casgevy to be the first of many future treatments that address a disease at its genetic cause through gene editing technology. According to GlobalData, as of November 16, 2023, over 175 trials have been initiated for gene editing products, trialing nearly 150 different novel treatments around the world.
Exca-cel was among the earliest programs to leverage the CRISP-Cas9 platform technology to treat an inherited rare disease, and the CRISPR approach is being taken to provide relief in a wide array of monogenic diseases. To name a few, trials are underway for:
- Inherited retinal diseases, such as retinitis pigmentosa
- Blood disorders, such as hemophilia
- Metabolic diseases, such as mucopolysaccharidoses
Gene editing is further being utilized for infectious diseases, such as HIV, and is being employed vigorously in oncology programs. In addition to sickle cell disease, exa-cel has also been developed for the treatment of transfusion-dependent b-thalassemia (TDT), and its Standard Review has a PDUFA target action date of March 30, 2024.
What Does the Future of Gene Editing Hold?
Gene editing has provided the key to moving autologous cellular immunotherapy, such as the CAR T products currently part of the standard of care, to an allogeneic modality. By using gene editing to turn off the triggers that can make it dangerous to transplant cells from one person to another, delivery of allogeneic cellular immunotherapy has the potential to reach a much wider proportion of the cancer patient community. Allogeneic products leverage cells from healthy donors rather than the patient’s own cells, which may have been damaged by chemotherapy, meaning allogeneic cancer immunotherapy could be delivered to patients sooner and with much less variability.
Thanks to the relentless progress of gene editing technologies, plus the continuing advancements in lipid nanoparticle technology, many of the newest investigational products for gene editing can be delivered directly to the patient rather than through modification of cells outside their body. While these cutting-edge approaches require and deserve thoughtful regulatory consideration, these advancements will relieve various logistical boundaries that have hampered development to date. As a result, future approved treatments will be more economical and scalable and, therefore, more accessible to the very patients we all seek to serve.
We absolutely celebrate this new treatment option coming soon to patients in the sickle cell disease community and the brighter future of gene editing to bring meaningful treatments to patients around the world.
Worldwide’s Cell and Gene Therapy Experience
Worldwide Clinical Trials is experienced in the delivery of full-service cell and gene therapy clinical trials at all phases across hematology, oncology, neurology, metabolic, ophthalmology, and cardiovascular indications, including both ex-vivo and in-vivo gene editing programs.
We understand that every cell and gene therapy is different, which is why we take a personalized approach to tackle your scientific, regulatory, and operational needs. Specializing in end-to-end solutions for adult and pediatric cell and gene therapy programs, our integrated teams are here to support your trial every step of the way. Learn more about our cell and gene therapy expertise today.



